.jpg)
Foodborne disease (FBD) is an important cause of morbidity and mortality in the United States. The Centers for Disease Control and Prevention (CDC) estimates that each year, approximately 1 in 6 Americans (or 48 million people) get sick, 128,000 are hospitalized, and 3000 die of FBD.[1] FBD can result from several causes, including preformed toxins, invasive or toxin-producing bacteria, viruses, parasites, and heavy metals. For example, in 2008-2009, peanut butter contaminated with Salmonella was responsible for hundreds of illnesses and several deaths.
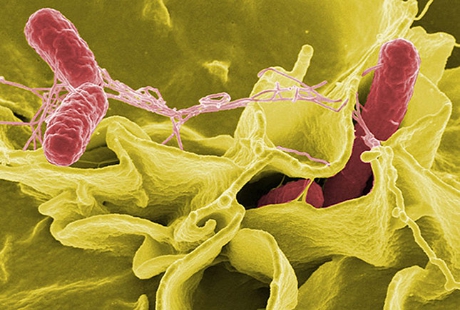
Salmonella enterocolitis is a diarrheal illness that is typically caused by contaminated food (most commonly beef, poultry, or eggs). After ingestion, Salmonella organisms attach and then invade the cells of the intestinal lumen, causing a massive efflux of fluid and electrolytes. The clinical presentation consists of large-volume watery diarrhea, fever, abdominal cramping, chills, headache, tenesmus, and myalgia. Diarrhea typically lasts for 3-7 days. Formal diagnosis is made by means of stool culture. The disease is typically self-limited, and treatment involves fluid and electrolyte replacement. Antibiotics do not shorten the duration of symptoms and may prolong the duration of convalescent carriage; they are thus reserved for patients at risk for invasive disease. The mortality associated with uncomplicated Salmonella enterocolitis is less than 1%, but if bacteremia develops, the mortality may increase to 20-30%.

The patient history is of particular importance in evaluation for suspected FBD. The patient should be asked about recent travel, consumption of suspect foods, recent antibiotic use, sick contacts, and details about abdominal pain (eg, location and character), vomitus (eg, bilious or bloody), and diarrhea (eg, watery, bloody, copious, foul-smelling, foamy, or greasy). Pictured is Escherichia coli, a gram-negative bacillus, on Gram staining. Different strains of E coli are frequently implicated in FBD. Enterotoxigenic strains are the most common cause of traveler's diarrhea; enteroinvasive strains cause febrile dysentery, and enterohemorrhagic strains, such as E coli O157:H7, cause hemorrhagic colitis with a risk for hemolytic-uremic syndrome (HUS), particularly in children.
A 35-year-old man presents with nausea, abdominal cramping, and headache that started while he was eating mahi mahi, sautéed spinach, and French fries at a restaurant. He denies experiencing any vomiting or diarrhea. On examination, he has B. Prolonged neurologic sequelae are common with this condition
C. Proper cooking of the fish would have prevented his illness
D. Proper washing of the spinach would have prevented his illness
E. The short incubation period is consistent with ingestion of a preformed toxin

Answer: E. The short incubation period is consistent with ingestion of a preformed toxin
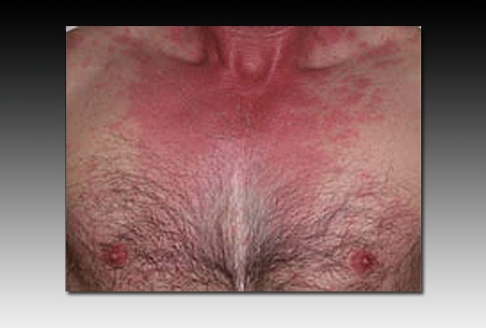
The short incubation period (10-30 minutes) and the clinical presentation are consistent with scombroid poisoning (currently more often referred to as histamine fish poisoning because many cases are caused by nonscombroid fish). Histamine fish poisoning results in gastrointestinal distress with nausea, abdominal cramping, and diarrhea and also features a distinctive flushing of the face and upper torso (shown). Other symptoms include palpitations and headache; a minority of patients may develop wheezing and hypotension. Histamine fish poisoning results from the consumption of fish that was inadequately refrigerated, resulting in bacterial production of biogenic amines and decarboxylation of histidine to histamine. Histamine is heat-stable and resists cooking. Spinach has been associated with outbreaks of FBD due to E coli, including E coliO157:H7; however, the short incubation period in this patient makes E coli an unlikely agent. Because histamine fish poisoning is due to ingestion of a preformed toxin, antibiotics are of no utility. The condition is self-limited, unlike ciguatera poisoning, which can feature prolonged neurologic sequelae.
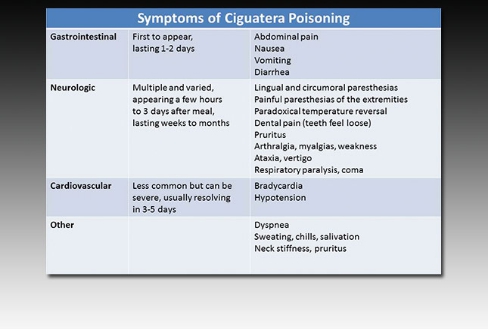
Ciguatera poisoning is an FBD associated with seafood consumption. It is caused by consumption of ciguatoxins produced by dinoflagellates that are present in tropical and subtropical waters. Ciguatoxins undergo biomagnification and may be present in high concentrations in carnivorous tropical and subtropical fish, such as grouper and amberjack. Ciguatera poisoning features both gastrointestinal and neurologic symptoms (shown). Cold allodynia, a burning sensation on exposure to cold, is highly suggestive of ciguatera poisoning.
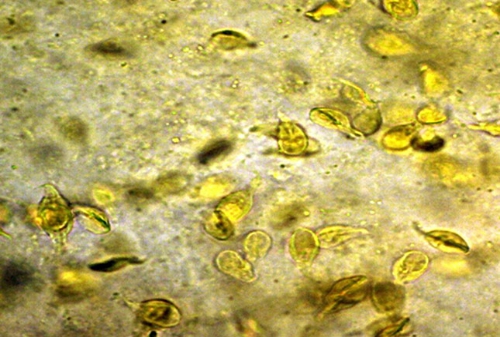
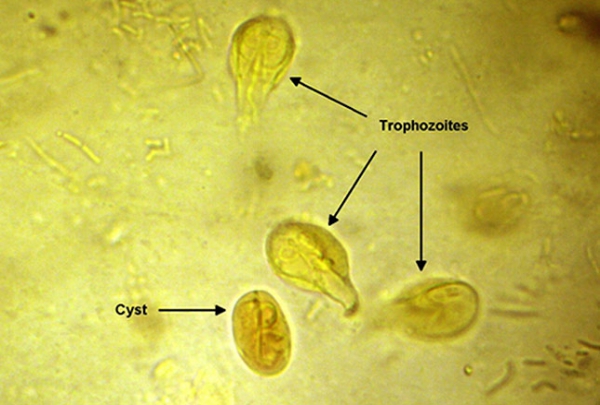
A 19-year-old man presents with diarrhea, fatigue, and weight loss of 5 lb, all of which have been present or developed over the past 2 months. He has no history of recent international travel, recent antibiotic use, nausea, vomiting, or abdominal pain. Stool studies are performed. A stool wet mount with iodine stain is pictured.
Which of the following statements about this man's condition is most accurate?
A. Bloody diarrhea is common owing to the invasive nature of the organism
B. Ciprofloxacin is first-line therapy for this condition
C. Transmission occurs via fecal-oral contamination
D. HIV testing should be performed to evaluate for immunocompromise
E. Mosquitos serve as a vector for the causative organism
Answer: C. Transmission occurs via fecal-oral contamination
Giardiasis is a common cause of diarrheal disease, both in the United States and throughout the world. Infection typically occurs from fecal-oral contamination, attributable either to poor hygiene or to sexual transmission. Consumption of contaminated water is another method of transmission. There are no vectors for Giardia, although humans and other mammals serve as reservoirs. Diarrheal stools are commonly described as malodorous or greasy (not bloody), and weight loss is common. Diagnosis may be made by means of enzyme-linked immunoassay of the stool or examination of the stool for ova and parasites, which may reveal Giardia lamblia cysts or trophozoites (shown). Metronidazole is first-line therapy. Giardiasis causes disease in immunocompetent patients, and testing for immunocompromise is not necessary.
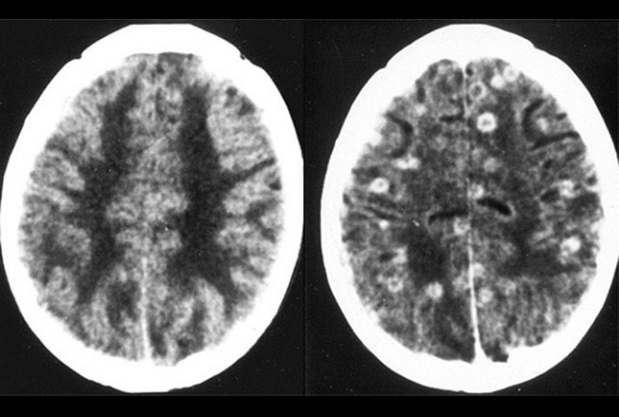
Cysticercosis is an uncommon FBD in the United States (approximately 1000 cases/year), but its incidence is increasing because of increased immigration from and travel to endemic areas (Mexico, Central and South America, Africa, India, and East Asia). Cysticercosis is due to fecal-oral transmission of Taenia solium eggs shed from a tapeworm host. T solium larvae (cysticerci) invade the gastrointestinal blood supply and are distributed throughout the body, resulting in the formation of cysts. The slide shows nonenhanced (left) and enhanced (right) CT scans of the head in a patient with neurocysticercosis, which may result in seizures, stroke, or hydrocephalus.

A 22-year-old male college student presents to the ED with severe nausea and vomiting. He just broke up with his girlfriend and reports that he has mainly been surviving on leftovers. He began to experience symptoms a couple of hours after digesting old fried rice.
Which of the following organisms is most likely to be responsible for his symptoms?
A. Bacillus cereus
B. Clostridium perfringens
C. Clostridium botulinum
D. E coli
Answer: A.
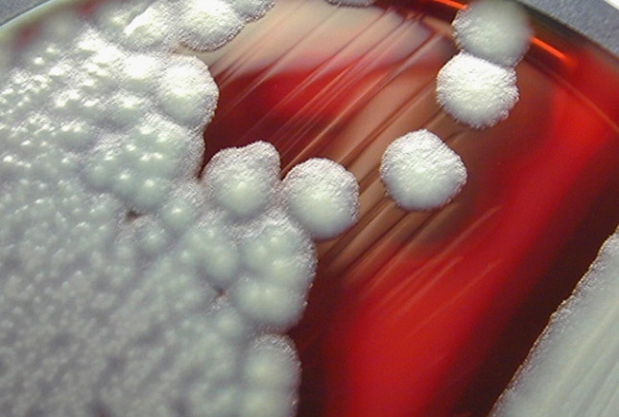
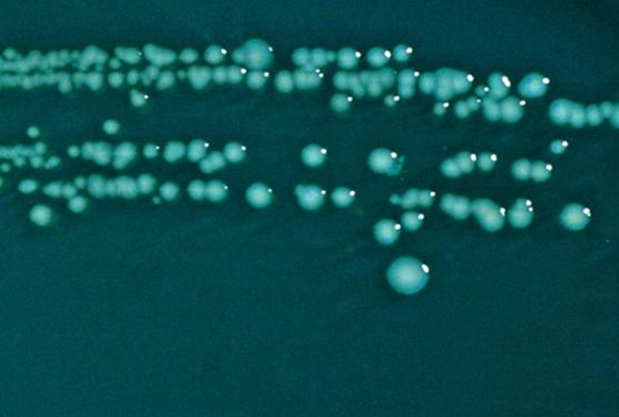
B cereus is a gram-positive aerobic bacterium that can cause FBD; it is most commonly associated with improperly cooked fried rice. B cereus produces endospores that are able to survive temperatures as high as 100°C. In foods that are improperly refrigerated, the endospores will readily germinate. Two specific forms of disease exist. In the diarrheal form, patients develop diarrhea and abdominal pain after an incubation period of roughly 12 hours. In the emetic form, which is usually associated with improperly cooked rice, enterotoxins induce nausea and vomiting within a couple of hours. Treatment is purely symptomatic, and most symptoms will resolve in 24 hours. The image shown demonstrates B cereus colonies growing on a sheep's-blood agar plate.
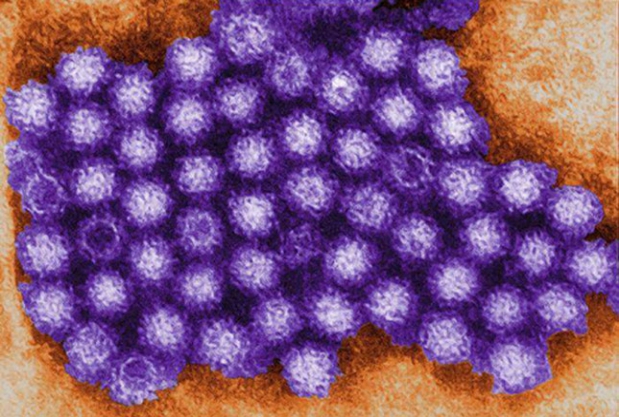
Norovirus, a genus of RNA viruses that includes Norwalk and Norwalk-like viruses, is responsible for roughly 50% of cases of FBD in the United States. Norovirus is usually transmitted via fecally contaminated food or water. It is highly resistant to freezing and can survive temperatures up to 60°C, as well as the use of chlorine, alcohol, and antiseptic hand solutions. Once norovirus enters the body, it causes damage to the microvilli in the small intestine, leading to profuse vomiting, watery diarrhea, low-grade fever, and malaise. Formal diagnosis is rarely ascertained but can be achieved with polymerase chain reaction assays. Treatment is generally supportive, and the disease is usually self-limited. Strict handwashing is imperative to prevent widespread outbreaks. A transmission electron micrograph of norovirus is shown.
Image courtesy of the Centers for Disease Control and Prevention (CDC).
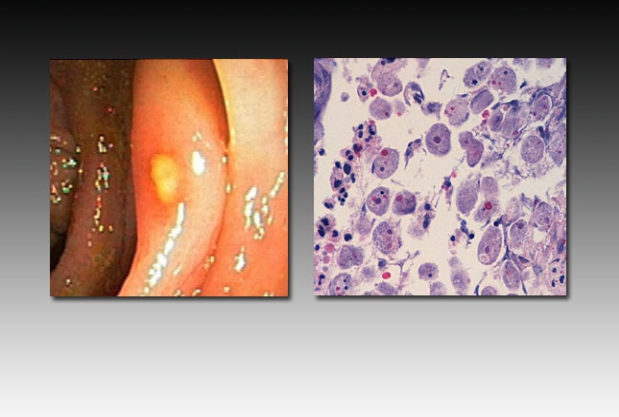
Amebic colitis is uncommonly encountered in the United States. Common symptoms include cramping, abdominal pain, and watery diarrhea. Risk factors include traveling to endemic areas (Africa, India, Mexico, and Central and South America), being an immigrant or refugee from endemic areas, being a man who has sex with men, and being exposed to institutions with poor sanitary conditions. Stool examination may demonstrate the parasite, although stool antigen studies are of higher sensitivity and specificity. The patient pictured above was referred for colonoscopy because he had abdominal pain and diarrhea for 3 months. Pictured on the left is an ulceration characteristic of Entamoeba histolytica; the wound has slightly heaped-up edges. Pictured on the right is a tissue biopsy sample from the same patient, showing numerous E histolytica trophozoites. Phagocytosed erythrocytes can be seen in many of the organisms.
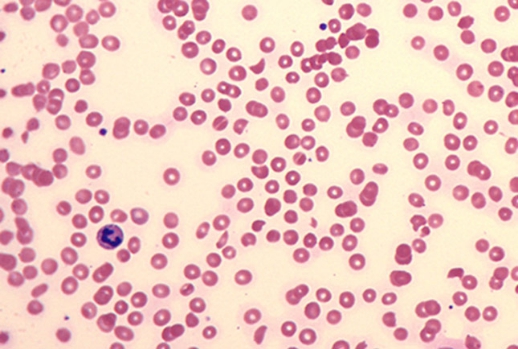
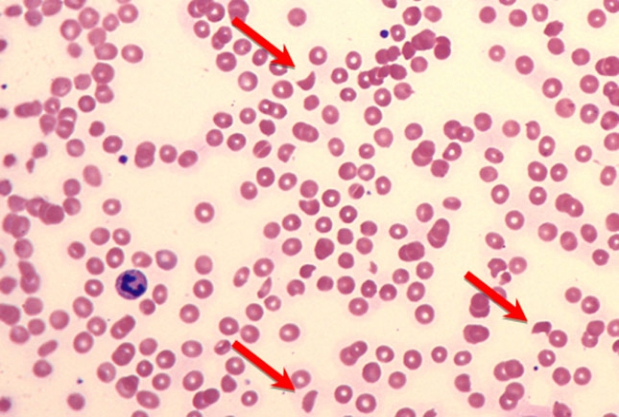
A 30-year-old man presents with several days of abdominal cramping, nausea, vomiting, bloody diarrhea, and lethargy. Urinalysis shows hematuria, and a complete blood count with peripheral blood smear is performed (shown). Findings suggest HUS.
Which of the following statements is most accurate?
A. The case-fatality rate for treated patients is greater than 50%
B. This condition occurs most frequently in persons aged 20-40 years
C. This condition is caused by ingestion of preformed toxins
D. This condition is the most common cause of acute renal failure in children
E. Reactive thrombocytosis is commonly encountered
Answer: D. This condition is the most common cause of renal failure in children
Colitis caused by Shiga toxin-producing E coli (STEC), such as E coli O157:H7, carries a risk for subsequent HUS. Between 1982 and 2002, 354 cases of E coli O157:H7-associated HUS were reported. HUS has a fatality rate of 3-5% in the United States, but the rate is as high as 72% in underdeveloped countries. HUS may occur at any age but is most common in children aged 7 months to 6 years and is the most common cause of acute renal failure in this age group. The peripheral blood smear pictured shows schistocytes (arrows) due to intravascular hemolysis and thrombocytopenia resulting from thrombocyte consumption, sequestration, and destruction.

Shellfish poisoning occurs when toxins produced by algae are concentrated in bivalve mollusks. Algal blooms, sometimes called "red tides" (pictured), are particularly associated with shellfish poisoning. There are 4 recognized types of shellfish poisoning, each of which is associated with a unique toxin or class of toxins: amnesic shellfish poisoning, diarrheal shellfish poisoning, neurotoxic shellfish poisoning, and paralytic shellfish poisoning.

Consumption of fish in the family Tetraodontidae (commonly known as pufferfish) can result in paralysis and death owing to tetrodotoxin, a sodium-channel blocker that is produced by symbiotic bacteria. In Japan, these fish are prized as a delicacy called fugu(pictured). The presence of small quantities of tetrodotoxin in the finished product produces a desired perioral tingling. To minimize the risk of toxicity and death, only trained and licensed chefs are allowed to prepare fugu. Poisoning may result from domestic preparation of the fish or surreptitious sale of the fish under another name (eg, salmon).
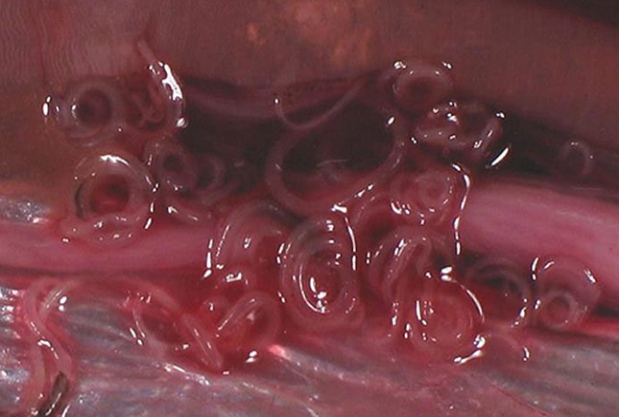
Anisakiasis is a rare cause of FBD in the United States; fewer than 10 cases occur annually. Symptoms include nausea, vomiting, and abdominal pain. Anisakiasis is caused by consumption of raw or undercooked fish containing larvae of the nematode Anisakis simplex. It is a more common cause of disease in areas where consumption of raw, pickled, or salted fish is common: for example, sushi in Japan and ceviche in Latin America. Infection can be prevented by adequate freezing of fish intended for raw consumption. Anisakid larvae in herring flesh are pictured.
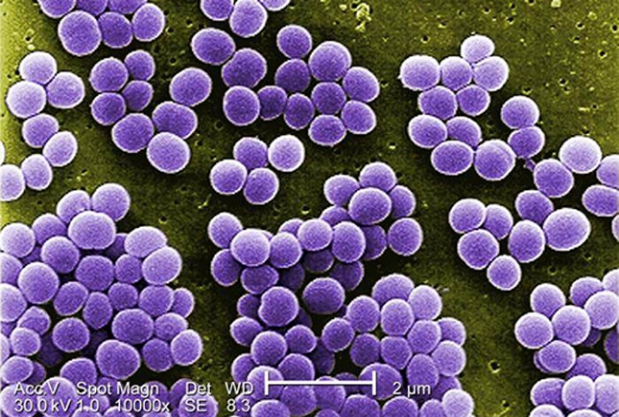
Staphylococcal enterotoxins are a common cause of FBD in the United States. Ingestion of enterotoxins produced by Staphylococcus in improperly refrigerated foods, such as picnic foods, puddings, and mayonnaise, results in FBD. Clinical presentation commonly features a short incubation period of 3-12 hours, followed by nausea, vomiting, and cramping abdominal pain with or without diarrhea; symptoms last 12-24 hours. Staphylococcal enterotoxins have superantigen properties and are associated with both menstrual and nonmenstrual toxic shock syndrome. Staphylococcal enterotoxin B (pictured) is categorized as a category B bioterrorism agent by the CDC.

A 4-month-old girl is brought to the ED by her parents for decreased activity and poor feeding. The parents note that the infant (shown) has not had a bowel movement in the past 24 hours. They deny feeding the infant honey, corn syrup, or home-canned foods but report having given her chamomile tea for colic 2 weeks previously.
Which of the following statements about the infant's condition is most accurate?
A. Antibiotic therapy should be initiated
B. Ascending paralysis has occurred as a consequence of demyelinating disease
C. Disease is caused by ingestion of preformed toxin
D. Nearby construction is a risk factor for disease
E. Therapy is limited to supportive care
Answer: D. Nearby construction is a risk factor for disease
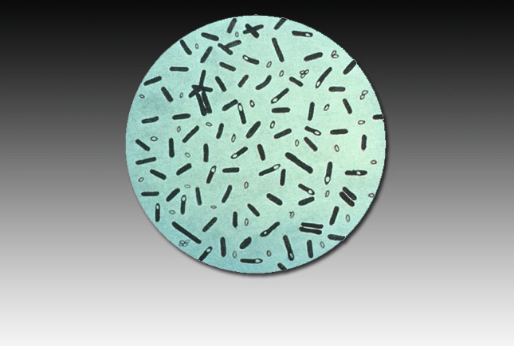
Whereas children and adults must ingest preformed toxin to develop clinical botulism, infant botulism (pictured) may occur after ingestion of Clostridium botulinum spores in unspoiled food (honey or corn syrup); toxins are produced in the infant's gut. Several cases of infant botulism due to chamomile tea ingestion have now been reported in the United States. Nearby construction is another risk factor, owing to soil disturbance. The incubation period of illness in this child (2-4 weeks) is consistent with infant botulism and not with foodborne botulism (incubation period, 18-36 hours), which is associated with improperly preserved foods. In either form of botulism, antibiotic therapy is contraindicated because it increases toxin release. Early therapy with human botulism immune globulin shortens hospital and ICU stays and reduces the need for mechanical ventilation or tube feeding. The photomicrograph shown demonstrates C botulinum stained with gentian violet.
Specialized agars can facilitate identification of the responsible agent in cases of suspected FBD. Pictured is Hektoen enteric agar, which is useful in the diagnosis of salmonellosis and shigellosis. This agar suppresses growth of gram-positive organisms and contains indicators for lactose fermentation and hydrogen sulfide production. E coliferments lactose, resulting in yellow-orange discoloration of the agar; Salmonella andShigella do not ferment lactose, resulting in green agar. Salmonella produces hydrogen sulfide, resulting in black discoloration of the bacterial colonies, whereas Shigella does not. The plate pictured, therefore, would be positive for Shigella.
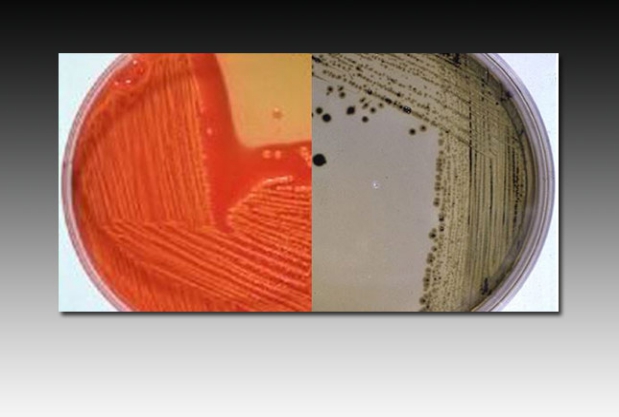
Pictured on this slide are two Hektoen enteric agar plates (the same agar pictured in the preceding slide). On the left, there is a yellow-orange discoloration due to a change in pH from a lactose fermenter, in this case E coli. On the right, the green background color indicates that the organism does not ferment lactose. Additionally, the blackish coloration of the colonies indicates the presence of ferric ammonium citrate indicator reacting with hydrogen sulfide produced by the bacteria, in this case Salmonella. This may be contrasted with the blue-green coloration of the Shigella colonies in the previous slide.